The artificial
hip joint
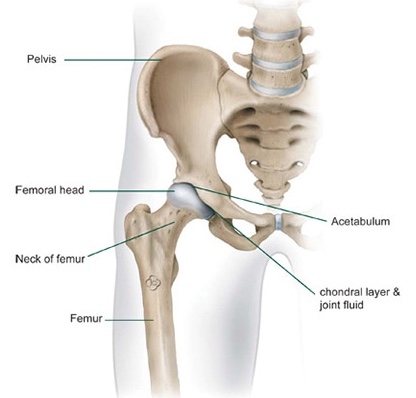
The structure of the hip joint
The hip joint is known as a ball and socket joint. The ball, which is called the femoral head, is found at the top of the thighbone or femur and the socket is a part of the pelvis called the acetabulum. In a healthy hip, the surfaces of these two bones (i.e. where they meet and actually form the joint) are covered in a layer of cartilage which allows for smooth, pain-free sliding. The joint is surrounded by a soft tissue envelope called the capsule which seals the joint and produces a fluid which nourishes, lubricates as well as enables smooth movement.

Arthritis or arthrosis of the hip joint
While wear and tear of the cartilage is by far the most common reason for hip replacement surgery, rheumatic conditions (rheumatoid arthritis) and fractures of the femoral neck (traumatic or age-related) are also quite common. The wear mentioned earlier is progressive and as such the joint becomes increasingly painful. Putting weight on it hurts more and walking distance reduces over time. Eventually even resting provides little relief from the pain.
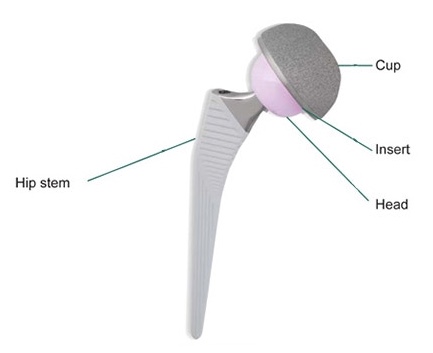
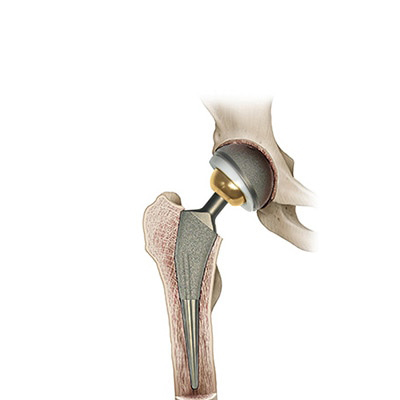
The replacement of the hip joint
Since the worn or damaged cartilage cannot be restored an arthritic hip is often replaced by artificial components. During the surgery the socket is almost always replaced first by a cup which is carefully wedged, screwed or cemented into the acetabulum of the pelvis. Then a stem is carefully wedged or cemented into the shaft of the thighbone. The artificial ball (or head) is attached to the top of this before being carefully maneuvered into the artificial socket (or cup). The choice of the hip prostheses depends largely on the patient’s bone quality, age, weight and anticipated activity levels. Most modern implants are made from specialised ceramics, metals and plastics.
The operation
The extent of the arthritis and suitability for replacement is determined via radiographs (or x-rays) beforehand. These images are also used for planning the surgery and any special equipment that may be needed. The procedure itself is totally pain-free whether it is done under a general anaesthetic (where the patient is unconscious) or under a spinal anaesthesia (where the patient is sedated but awake). Surgery times vary but typically range from 50 minutes to 120 minutes. Once in the operating room, the joint is opened (or exposed) and dislocated. The femoral neck is cut so that the worn ball (or femoral head) with its damaged painful cartilage can be removed. This creates enough space for the surgeon to remove the damaged cartilage in the socket or acetabulum. Small bony deformities can also be removed at this stage. Then the socket is replaced with a plastic cup which is either cemented into place or else a metal cup is carefully wedged into the prepared acetabulum and a plastic or ceramic liner is secured inside this. The shaft of the thighbone (or femur) is then prepared for the stem which is also carefully cemented or wedged into position. A metal or ceramic ball (or femoral head) is subsequently attached to the top of the stem. Once the ball is placed within the socket soft tissue tension is checked as well as the mobility of the new joint. Afterwards, the tissue is closed with sutures and a drain (which is removed 2-4 days later) for the wound secretions may also be inserted. The skin stitches or staples are removed after 12 to 14 days.
Possible complications
Blood loss during and after surgery is possible with any major procedure so sometimes a blood transfusion is necessary. Usually however, blood salvaging techniques (and systems like Cellsaver) are used for re-infusion. Here any lost blood is collected, cleaned and returned to the patient thus minimising the need for donated blood. In this way the risk of becoming infected with hepatitis or HIV and AIDS can be significantly reduced. Damage to large blood vessels and nerves also cannot be ruled out. For those patients who cannot be fully mobilised soon after their operation, a greater risk of deep vein thrombosis (DVT) exists. This danger is managed with physiotherapy as well as via the use of antithrombotic stockings and blood-thinning medication.
As far as the complications that are specific to the hip replacement itself are concerned, the most common ones are: fractures during the surgery, dislocation, differences in leg length, infection and loosening over time.
Postoperative care
Exercise is introduced on the first day after the operation as the risk of complications is lowered by this early mobilisation. Should a cemented prosthesis be implanted, the leg can immediately accept the patient’s full weight; in the case of a cementless implantation, the operated leg may only take partial body weight for a period of approximately six weeks. The extent of movement is limited however, for example in the first few weeks after hip joint replacement, certain rotating motions and crossing of the legs must be avoided. Intensive physiotherapy promotes the mobility and structure of the muscles. The rehabilitation measures jointly co-ordinated by the surgeon and the physiotherapist are of great importance in order for the operation to be successful and for the patient to make a rapid recovery. The active cooperation of the patient greatly assists in the fast achievement of this goal.